Swab your vagina for science: designing a diagnostic test for human papillomavirus, for use in low resource settings
By LifETIME CDT Student: Ella Boswell (She/Her) (University of Glasgow)
What’s my project about?
Human papillomavirus, also known as HPV, is very common, but certain strains cause cervical cancer. Low-cost, quick, and easy-to-use tests – similar to the covid lateral flow tests – are required to diagnose people in areas that don’t have access to labs. Nucleic acid amplification tests (NAATs) are techniques that involve taking a sample (of human blood, for example), and searching to see whether the DNA or RNA of a disease is present. This is done by adding primers, which are chemicals that are specific to the disease, as well as some other chemicals, to a reaction, holding the reaction at 65 degrees C for 30 minutes, and then putting the contents of the reaction onto a lateral flow strip, whose line goes red if the DNA or RNA of the disease is present. Loop-mediation isothermal amplification (LAMP) is a type of NAAT that is well-suited for use in places without labs because it functions at a single temperature, rather than needing different temperatures, as many NAATs do. I’m designing a test for HPV, using a NAAT, for use in rural parts of sub-Saharan Africa. A key challenge to be overcome is that there are over 200 types of HPV, but only 14 types that cause cervical cancer – so, the test must detect ‘high-risk’ types only.
How am I going to do that?
I’ll start by designing a test that works in the lab, for one type of HPV (HPV16), and I’ll test it on real samples from people who have had HPV. I’ll then ‘miniaturize’ the test, so it works in a device that’s about the size of your hand. I’ll take this to the field – in Kenya, probably – and test it amongst the population that it’s intended to be used by.
Meanwhile, I’ll be working on designing a test that targets the other 13 high-risk types. I’ll probably use CRISPR (alongside LAMP), which is a technology that can recognize extremely specific DNA sequences (and, so, distinguish between different types of HPV). You may have heard of CRISPR in some of the big debates around GMO foods, or ‘designer babies’ – it’s similar technology. I’ll add this test to the original device, and then test the whole thing in the field one final time.
Why does this matter?
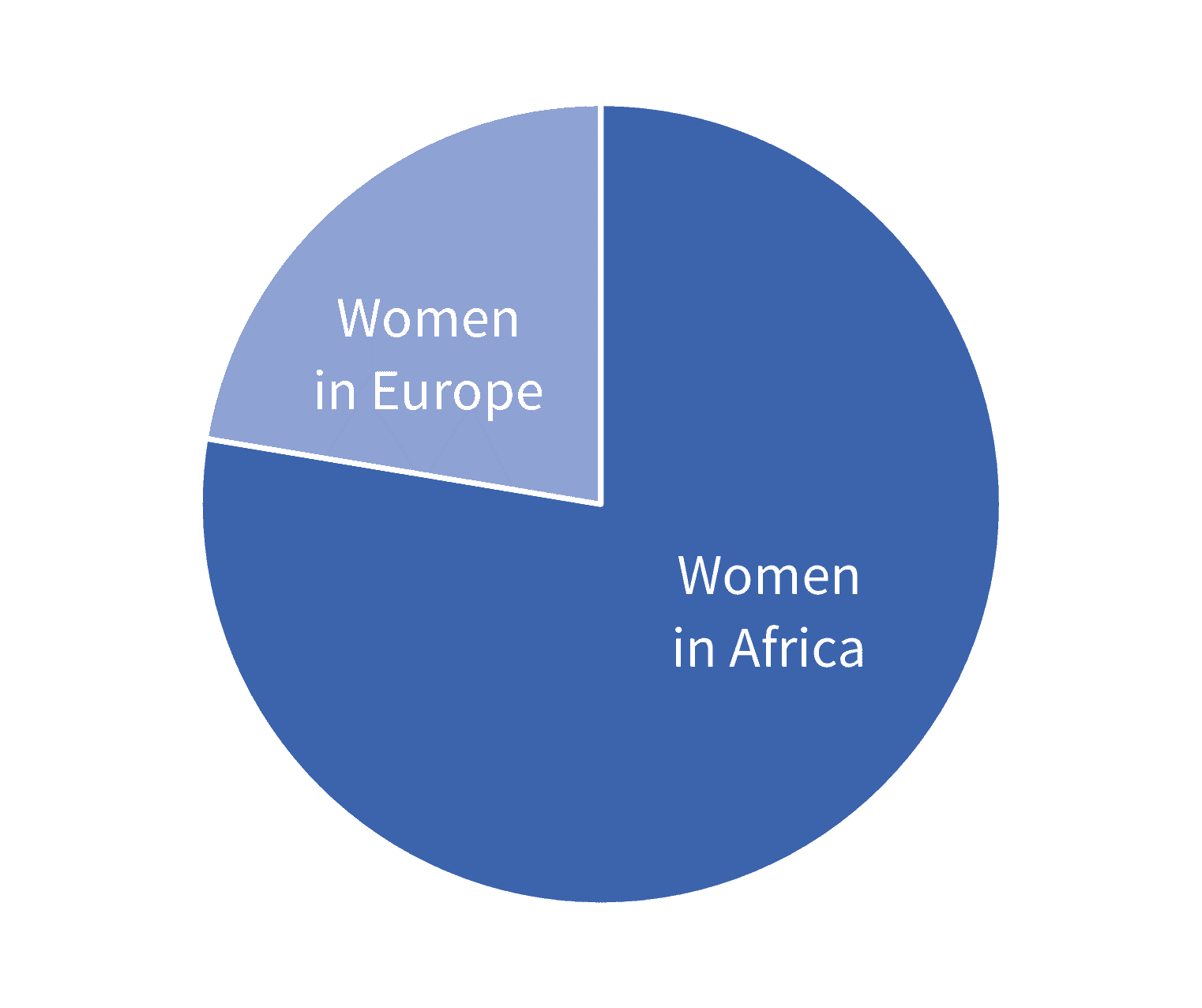
In 2018, cervical cancer – nearly always caused by human papillomavirus (HPV) – was the fourth most common cancer in women, with people in low-resource settings more frequently affected. The standard way to test whether or not you have cervical cancer is by undertaking cervical smear tests also known as a pap smear. Perhaps you’ve even had one of these tests – in the UK, they’re routinely offered to all women once they turn 25, and repeated every five years (assuming the test is negative). If the test is positive, you’d be referred to have follow-up tests and treatment. Since cervical smears require a trained professional to take a swab from the cervix, and lab infrastructure to receive the test, they’re not suitable for use in low-resource settings. In order to provide healthcare for everyone, a test needs to be developed that doesn’t require these things.